Track Co-Chair:
Mary Relling, St. Jude
Pharmacists have long recognized that using unique patient characteristics to guide pharmacotherapy decision-making can improve drug response and mitigate drug-associated risks. Age, weight, and dietary habits were among the first patient-specific characteristics used to individualize pharmacotherapy. As technologies advanced, analytic tools that measure surrogate markers of liver and renal function, together with drug concentrations in biological fluids, were adopted to optimize therapeutic regimens. Cutting-edge genomic technologies are now being integrated into patient care for the selection of targeted therapies and identification of those at increased risk of poor pharmacotherapy outcomes. We’re excited to bring together experts who are advancing pharmacogenomics at scale through cutting edge clinical implementation, research, and education.
- PMWC 2023 PGx Award Ceremony:
Pioneer Honoree: Dan Roden, Vanderbilt University Medical Center
Luminary Honoree: Kelly E. Caudle, St. Jude
- Fireside Chat:
PMWC 2023 Pioneer Honoree Dan Roden, Vanderbilt University Medical Center with Mary Relling, St. Jude - Keynote by PMWC 2023 Luminary Honoree:
- Kelly E. Caudle, St. Jude - Fireside Chat:
Chair: Damon Hostin, Illumina
- Howard McLeod, Intermountain Health - Laboratory Testing and Reports
Chair: Kristy Crooks, University of Colorado
- Ann M. Moyer, Mayo Clinic
- Stuart Scott, Stanford University
- Implementation of PGx at UCSF
- Bani Tamraz, UCSF
- From Economics to Reimbursement (PANEL)
Chair: Sara Rogers, American Society of Pharmacovigilance
- Stirling Bryan, The University of British Columbia
- Ray Stultz, Optum
- Gabriel Bien-Willner, Palmetto GBA
- Policy Efforts to Address Barriers to PGx Adoption
Chair: Kristine Ashcraft, Invitae
- Pam Traxel, ACS CAN - PGx Practice Liability
Chair: Dan Hertz, University of Michigan
- Anthony Morreale, VA, San Diego
- Karen Merritt, Patient Advocate - Diversity, Equity, and Inclusion in Pharmacogenomics Implementation
- Carlos Bustamante, Galatea Bio
- Kathy Giacomini, UCSF - Implementation of PGx Program & PGx Clinic Services in a Large Rural Healthcare Setting
- April Schultz, Sanford
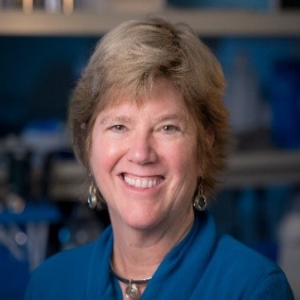
Session Chair Profile
Biography
Dr. Relling has been a pioneer in both the science and clinical application of pharmacogenomics. Her research has resulted in seminal laboratory discoveries that unraveled the mechanisms of drug-induced adverse effects, and the integration of biologic, genomic, and pharmacologic discoveries into comprehensive clinical protocols, leading to improved cure rates for children with acute lymphoblastic leukemia. In recognition for her work she was elected to the Institute of Medicine (now National Academies of Medicine) in 2009 and received the Pediatric Oncology Award from ASCO. Mary has been recognized by the American Society for Clinical Pharmacology and Therapeutics. Mary, along with Dr. Teri Klein of Stanford, co-founded the Clinical Pharmacogenomics Implementation Consortium (CPIC) that has published pharmacogenetic guidelines for over sixty-five medications. These guidelines are now implemented around the globe. Mary received her Bachelor of Science degree from the University of Arizona and her PharmD from the University of Utah College of Pharmacy.
Session Chair Profile
Biography
Kristine Ashcraft is a molecular biologist by training and is the former CEO and founder of YouScript, recently acquired by Invitae. She has worked in pharmacogenomics since 2000 and was named one of the 25 leading voices in precision medicine. She serves on the STRIPE Steering Committee, the FDA collaborative community for pharmacogenomics. Kristine has authored multiple publications on the clinical and economic benefits of pharmacogenomic testing including one lauded as one of the most influential publications at an American Medical Informatics Association meeting. She has been interviewed by numerous media outlets including the New York Times, the Wall Street Journal, and NBC Nightly News and has spoken at SXSW, American Society of Human Genetics, and numerous precision medicine conferences. She is committed to catalyzing the adoption of precision medicine.
Talk
A discussion of federal and state policy efforts to address known barriers to PGx adoption such as reimbursement, education, and healthcare IT infrastructure including the Right Drug Dose Now Act and American Cancer Societys state biomarker testing bills.
Session Chair Profile
Biography
Dr. Crooks is a board-certified clinical molecular and cytogeneticist and Director of the Colorado Center for Personalized Medicine (CCPM) Biobank, an institutional initiative for the development of sample cohorts and genetic and health record datasets for research and clinical use. With over 200,000 participants from across the United States, the CAP-accredited CCPM Biobank represents one of the largest and most diverse clinical biorepository cohorts generated to date. Dr. Crooks’ primary research interests include evaluating metrics of population-based genetic screening and return of clinically-actionable genetic test results, including pharmacogenetics and high-impact pathogenic constitutional variants, to advance precision medicine and improve patient outcomes.
Session Chair Profile
Biography
Sara Rogers co-founded the American Society of Pharmacovigilance and co-led the formation of the Standardizing Laboratory Practices in Pharmacogenomics (STRIPE) Collaborative Community, a public-private multidisciplinary initiative to develop consensus-based industry standards for pharmacogenetics testing. She joined Texas A&M University in 2021, where she holds joint appointments with Institute of Biosciences and Technology, School of Medicine and Irma Lerma Rangel School of Pharmacy. Rogers co-chairs the Pharmacogenomics Access and Reimbursement Coalition and collaboratively develops the Coalition’s research agenda to understand the payment and policy landscape for pharmacogenetics testing and its role in disparities in patient access. Rogers is an organizational member of the NIH NHGRI Inter-Society Coordinating Committee and develops educational resources to help practitioners navigate coverage for pharmacogenetics testing. Rogers has served as co-investigator for a pilot study to identify ethical values and priorities related to pharmacogenomics. Her research focuses extensively on patient access to and reimbursement for pharmacogenetics testing.
Talk
While innovative precision technologies can improve patient outcomes; they present new information and price shocks to payers. Emerging clinical guidelines may add to the confusion and further hamper payer acceptance. During this session, we’ll explore payer perspectives in the evidence evaluation processes that guide coverage decisions.
Speaker Profile
Biography
Dr. Scott is a Professor in the Department of Pathology at Stanford University and Director of the Stanford Medicine Clinical Genomics Laboratory, where he oversees genomic test innovation and implementation. In addition, Dr. Scott is certified by the American Board of Medical Genetics and Genomics (ABMGG) in Clinical Molecular Genetics and Genomics, and Clinical Cytogenetics, and his research interests include human genomics, pharmacogenomics, cytogenomics, long-read sequencing, and the implementation of genomic medicine. He is a member of the Clinical Pharmacogenetics Implementation Consortium (CPIC), PharmGKB, PharmCAT, PharmVar, AMP Pharmacogenomics Working Group, International Union of Basic and Clinical Pharmacology (IUPHAR), and other national human genomics consortia (ClinGen, UDN, GREGoR). He has co-authored several CPIC practice guidelines and has published over 140 peer-reviewed manuscripts and book chapters on clinical genomics, pharmacogenomics, and genomic medicine implementation.
Talk
Clinical Pharmacogenomic Testing: Sequencing Innovations and Reporting
This presentation will discuss innovative sequencing solutions for clinical pharmacogenomic testing, as well as provide an overview of clinical pharmacogenomic reporting best practices.
Speaker Profile
Biography
Dr. Morreale has been entrusted with organizing, standardizing and expanding the scope of clinical pharmacy practice nationally since 2010. In recent years this has included the integration of pharmacogenomics into clinical practice for pharmacists in all practice settings. In 2018 he took on the added responsibility of overseeing national policy development and maintenance for the which also involves developing and implementing practice changes, policy, regulations and guidance. Prior to this national position he served as Chief and Associate Chief of Pharmacy for a large Healthcare System and its satellite facilities for nearly 20 year giving him a great deal of experiencing in running and managing a highly complex pharmacy organization. He is well versed in the legal, regulatory, and operational aspects and challenges facing such organizations.
Talk
Integration of pharmacogenomic (PGx) testing into clinical practice has accelerated, moving it from a novelty to a standard part of patient care. As PGx testing becomes a standard of care, failure to integrate it into patient care practice could lead to instances where care may not be optimized, raising potential malpractice issues.
Speaker Profile
Biography
Dr. Ann Moyer is an Associate Professor of Laboratory Medicine and Pathology as well as Assistant Professor of Pharmacology at the Mayo Clinic where she is involved in clinical laboratory testing for pharmacogenomics and hereditary disorders. She is the Vice Chair for Quality of the Division of Laboratory Genetics and Genomics. Her research interests include pharmacogenomics (particularly improvements in clinical laboratory testing and impact of rare variants), complement system genetics, and primary immunodeficiency genetics. Dr. Moyer has authored over 80 peer-reviewed manuscripts. After graduation from the University of Wisconsin-Platteville, Dr. Moyer completed the MD/PhD program, pathology residency, and molecular genetic pathology fellowship at Mayo Clinic. Her PhD thesis work focused on the pharmacogenomics of phase II drug metabolizing enzymes under the mentorship of Dr. Richard Weinshilboum.
Talk
Pharmacogenomics Laboratory Best Practices and Navigating Regulatory Requirements
This presentation will cover considerations and resources for developing and running a clinical test, including a brief discussion of the regulatory framework.
Speaker Profile
Biography
In 2003, Dan Roden, MD, then director of the Division of Clinical Pharmacology at
Vanderbilt University Medical Center, imagined a large-scale biobank integrated with
electronic health records to help doctors “personalize” medical care for their patients. That
vision became BioVU, today one of the world’s largest bio-banks, with over 300,000 DNA
samples from a single health care system. In its 15th year, BioVU has enabled hundreds of
studies and publications exploring the genetic underpinnings of a host of conditions
including cancer, heart disease, and diabetes, and the development of new tools like
PheWAS. Since joining the Vanderbilt faculty in 1981, Dr. Roden has become
internationally recognized for his studies of the mechanisms and treatment of abnormal
heart rhythms and variability in drug response. One major interest has been
pharmacogenomics, and especially the role genetic variations play in adverse drug
reactions such as drug-induced arrhythmias. He directed the Division of Clinical
Pharmacology from 1992 to 2004 when he became founding director of the Oates Institute
for Experimental Therapeutics. In 2016, a concerted effort was made to obtain genotyping
data from a large cohort of the BioVU samples. About 90,000 samples were genotyped. All
genomic data becomes available to VUMC-affiliated researchers studies can often be done
without the need for additional genotyping. Researchers can also look through the de-
identified version of the EHR and request that certain samples be genotyped. Dr. Roden is
a fellow of the American Association for the Advancement of Science, and has been elected
to membership in the American Society for Clinical Investigation and the Association of
American Physicians. Roden has authored more than 700 peer-reviewed scientific papers.
He is a leader in VUMC’s PREDICT project (Pharmacogenomic Resource for Enhanced
Decisions in Care and Treatment), which since 2010 has applied genomic testing to drug
prescribing, in an effort to avoid adverse drug reactions. He co-directed the Vanderbilt site
of the Pharmacogenetics Research Network funded by the National Institutes of Health
(NIH) 2001-2021, and is co-principal investigator for the VUMC site of the NIH Electronic
Medical Records and Genomics (eMERGE) Network and the NIH All of Us program’s Data
and Research Center. Dr. Roden received his medical degree from McGill University and
undertook Fellowships in both Clinical Pharmacology and Cardiology at Vanderbilt
Speaker Profile
Biography
The Clinical Pharmacogenetics Implementation Consortium (CPIC®) is an international consortium of volunteers and a small, dedicated staff who are interested in facilitating the use of pharmacogenetic tests results for patient care. One barrier to implementation of pharmacogenetic testing in the clinic is the difficulty in translating genetic laboratory test results into actionable prescribing decisions for affected drugs. CPIC’s goal is to address this barrier to clinical implementation of pharmacogenetic tests by creating, curating, and posting freely available, peer-reviewed, evidence-based, updatable, and detailed gene/drug clinical practice guidelines publications. To date, CPIC has published 26 gene-based clinical guidelines. CPIC guidelines follow standardized formats, include systematic grading of evidence and clinical recommendations, use standardized terminology, are peer-reviewed, and are published in a leading journal (in partnership with Clinical Pharmacology and Therapeutics) with simultaneous posting to cpicpgx.org, where they are regularly updated. CPIC started as a shared project between PharmGKB, and the Pharmacogenomics Research Network (PGRN) in 2009. CPIC guidelines are indexed in PubMed as clinical guidelines, endorsed by ASHP and ASCPT, and referenced in ClinGen and PharmGKB. Dr. Caudle oversees all Clinical Pharmacogenomic implementation Consortium-related projects and the CPIC guideline development process including the coordination of the guideline-writing committees, the guideline evidence reviews, and the writing of the guideline manuscript and supplement. Dr. Caudle is also involved in clinical implementation of pharmacogenetics at St. Jude Children’s Research Hospital. She has published over 50 manuscripts in the area of pharmacogenomics. Dr. Caudle received a bachelor of science from Middle Tennessee State University and her Pharm D and PhD in Pharmaceutical Sciences from University of Tennessee Health Science Center where she is currently an affiliate Asst. Professor. She has completed an ASHP-accredited PGY2 residency at Le Bonheur Children’s Hospital and is a board‐certified Pharmacotherapy Specialist.
Talk
CPIC: Advancing Pharmacogenomics into Routine Clinical Practice
Over the past 12 years, the Clinical Pharmacogenetics Implementation Consortium (CPIC) has provided resources to facilitate the implementation of pharmacogenetics into routine clinical practice. To date, CPIC has published 26 gene-based clinical guidelines covering 25 genes and over 90 drugs. This talk will explore the past, present and future of CPIC.
Speaker Profile
Biography
Pam is responsible for helping ACS CAN develop relationships with companies and individuals to help further the fight against cancer through dynamic partnerships, events, and forums. Pam began her career with ACS CAN in 2007. She has been integrally involved in helping to establish ACS CAN as a nationwide advocacy organization that influences and shapes public policy at all levels of government to impact our mission and to represent the voices of all cancer patients and their families.
Speaker Profile
Biography
In 2003, Dan Roden, MD, then director of the Division of Clinical Pharmacology at Vanderbilt University Medical Center, imagined a large-scale biobank integrated with electronic health records to help doctors “personalize” medical care for their patients. That vision became BioVU, today one of the world’s largest bio-banks, with over 300,000 DNA samples from a single health care system. In its 15th year, BioVU has enabled hundreds of studies and publications exploring the genetic underpinnings of a host of conditions including cancer, heart disease, and diabetes, and the development of new tools like PheWAS. Since joining the Vanderbilt faculty in 1981, Dr. Roden has become internationally recognized for his studies of the mechanisms and treatment of abnormal heart rhythms and variability in drug response. One major interest has been pharmacogenomics, and especially the role genetic variations play in adverse drug reactions such as drug-induced arrhythmias. He directed the Division of Clinical Pharmacology from 1992 to 2004 when he became founding director of the Oates Institute for Experimental Therapeutics. In 2016, a concerted effort was made to obtain genotyping data from a large cohort of the BioVU samples. About 90,000 samples were genotyped. All genomic data becomes available to VUMC-affiliated researchers studies can often be done without the need for additional genotyping. Researchers can also look through the de- identified version of the EHR and request that certain samples be genotyped. Dr. Roden is a fellow of the American Association for the Advancement of Science, and has been elected to membership in the American Society for Clinical Investigation and the Association of American Physicians. Roden has authored more than 700 peer-reviewed scientific papers. He is a leader in VUMC’s PREDICT project (Pharmacogenomic Resource for Enhanced Decisions in Care and Treatment), which since 2010 has applied genomic testing to drug prescribing, in an effort to avoid adverse drug reactions. He co-directed the Vanderbilt site of the Pharmacogenetics Research Network funded by the National Institutes of Health (NIH) 2001-2021, and is co-principal investigator for the VUMC site of the NIH Electronic Medical Records and Genomics (eMERGE) Network and the NIH All of Us program’s Data and Research Center. Dr. Roden received his medical degree from McGill University and undertook Fellowships in both Clinical Pharmacology and Cardiology at Vanderbilt
Speaker Profile
Biography
Focused on genomics technology and its application in medicine, agriculture, and evolutionary biology. I was Founding Director (with Marc Feldman) of the Center for Computational, Evolutionary, and Human Genomics. I serve as an advisor to the US federal government, private companies, startups, and non-profits in the areas of computational genomics, population and medical genetics, veterinary and plant genomics, and business strategy.
Session Chair Profile
Biography
Academic researcher focusing in cancer biomarkers including pharmacogenetics, with particular interest in chemotherapy-induced peripheral neuropathy and clinical uptake of pre-treatment DPYD testing.
Speaker Profile
Biography
Dr. Bien-Willner is the Medical Director of the MolDX program at Palmetto GBA, a Medicare Administrative Contractor (MAC). He is a leader in the Precision Medicine space and practices as a Board-certified Anatomic Pathologist and Molecular Genetic Pathologist. Throughout his career, he has been active in research, development, and advancement of molecular diagnostic services, specifically next generation sequencing. He has worked closely with clinicians to develop clear clinical diagnostic and treatment pathways directing Precision Medicine programs for community cancer centers. Dr. Bien-Willner received his MD and PhD degrees from Baylor College of Medicine, with a PhD in Human Molecular Genetics. He completed his residency, fellowship, and attained a faculty appointment at Washington University in St. Louis prior to leadership roles in laboratory and biotech companies before joining Palmetto GBA.
Speaker Profile
Biography
Karen Merritt is an impassioned patient advocate. Having lost her mother in 2014 after fatal toxicity from 5-FU chemotherapy due to an unknown DPD Deficiency, Karen is dedicated to advocating for pretesting for DPD Deficiency before fluoropyrimidine chemotherapy administration. Founding member of Advocates for Universal DPD/DPYD Testing (AUDT). As a Patient Representative, Karen is a member of ClinGen PGx Working Group as well as Standardizing Laboratory Practices in Pharmacogenomics (STRIPE)
Talk
Human Cost of Ignoring DPD Deficiency
Demonstrated clinical benefits show pretreatment DPYD testing increases patient safety, improves quality of care and saves money. Tragic to lose a loved one to cancer, but even more tragic when the death could have been prevented with a simple cheek swab. Time to pretest for DPD Deficiency.
Speaker Profile
Biography
The Clinical Pharmacogenetics Implementation Consortium (CPIC®) is an international consortium of volunteers and a small, dedicated staff who are interested in facilitating the use of pharmacogenetic tests results for patient care. One barrier to implementation of pharmacogenetic testing in the clinic is the difficulty in translating genetic laboratory test results into actionable prescribing decisions for affected drugs. CPIC’s goal is to address this barrier to clinical implementation of pharmacogenetic tests by creating, curating, and posting freely available, peer-reviewed, evidence-based, updatable, and detailed gene/drug clinical practice guidelines publications. To date, CPIC has published 26 gene-based clinical guidelines. CPIC guidelines follow standardized formats, include systematic grading of evidence and clinical recommendations, use standardized terminology, are peer-reviewed, and are published in a leading journal (in partnership with Clinical Pharmacology and Therapeutics) with simultaneous posting to cpicpgx.org, where they are regularly updated. CPIC started as a shared project between PharmGKB, and the Pharmacogenomics Research Network (PGRN) in 2009. CPIC guidelines are indexed in PubMed as clinical guidelines, endorsed by ASHP and ASCPT, and referenced in ClinGen and PharmGKB. Dr. Caudle oversees all Clinical Pharmacogenomic implementation Consortium-related projects and the CPIC guideline development process including the coordination of the guideline-writing committees, the guideline evidence reviews, and the writing of the guideline manuscript and supplement. Dr. Caudle is also involved in clinical implementation of pharmacogenetics at St. Jude Children’s Research Hospital. She has published over 50 manuscripts in the area of pharmacogenomics. Dr. Caudle received a bachelor of science from Middle Tennessee State University and her Pharm D and PhD in Pharmaceutical Sciences from University of Tennessee Health Science Center where she is currently an affiliate Asst. Professor. She has completed an ASHP-accredited PGY2 residency at Le Bonheur Children’s Hospital and is a board‐certified Pharmacotherapy Specialist.
Session Chair Profile
Biography
Focused on genomics technology and its application in medicine, agriculture, and evolutionary biology. I was Founding Director (with Marc Feldman) of the Center for Computational, Evolutionary, and Human Genomics. I serve as an advisor to the US federal government, private companies, startups, and non-profits in the areas of computational genomics, population and medical genetics, veterinary and plant genomics, and business strategy.
Talk
How Do We Enable Precision Health at Scale for All
Speaker Profile
Biography
In 2003, Dan Roden, MD, then director of the Division of Clinical Pharmacology at Vanderbilt University Medical Center, imagined a large-scale biobank integrated with electronic health records to help doctors “personalize” medical care for their patients. That vision became BioVU, today one of the world’s largest bio-banks, with over 300,000 DNA samples from a single health care system. In its 15th year, BioVU has enabled hundreds of studies and publications exploring the genetic underpinnings of a host of conditions including cancer, heart disease, and diabetes, and the development of new tools like PheWAS. Since joining the Vanderbilt faculty in 1981, Dr. Roden has become internationally recognized for his studies of the mechanisms and treatment of abnormal heart rhythms and variability in drug response. One major interest has been pharmacogenomics, and especially the role genetic variations play in adverse drug reactions such as drug-induced arrhythmias. He directed the Division of Clinical Pharmacology from 1992 to 2004 when he became founding director of the Oates Institute for Experimental Therapeutics. In 2016, a concerted effort was made to obtain genotyping data from a large cohort of the BioVU samples. About 90,000 samples were genotyped. All genomic data becomes available to VUMC-affiliated researchers studies can often be done without the need for additional genotyping. Researchers can also look through the de- identified version of the EHR and request that certain samples be genotyped. Dr. Roden is a fellow of the American Association for the Advancement of Science, and has been elected to membership in the American Society for Clinical Investigation and the Association of American Physicians. Roden has authored more than 700 peer-reviewed scientific papers. He is a leader in VUMC’s PREDICT project (Pharmacogenomic Resource for Enhanced Decisions in Care and Treatment), which since 2010 has applied genomic testing to drug prescribing, in an effort to avoid adverse drug reactions. He co-directed the Vanderbilt site of the Pharmacogenetics Research Network funded by the National Institutes of Health (NIH) 2001-2021, and is co-principal investigator for the VUMC site of the NIH Electronic Medical Records and Genomics (eMERGE) Network and the NIH All of Us program’s Data and Research Center. Dr. Roden received his medical degree from McGill University and undertook Fellowships in both Clinical Pharmacology and Cardiology at Vanderbilt
Speaker Profile
Biography
Dr. Giacomini is a world-renowned pharmacologist with many years of research experience focused on transporter biology and pharmacogenomics. Her research is focused on influx transporters, particularly influx transporters involved in drug disposition and targeting. In the early 2000s, she began a comprehensive research program focused on pharmacogenomics of membrane transporters and published many papers ranging from functional genomics of transporter polymorphisms to clinical studies elucidating the role of transporter polymorphisms on clinical drug response. Dr. Giacomini is also the Co-Principal Investigator of the UCSF-Stanford Center of Excellence in Regulatory Sciences and Innovation (CERSI), a major center funded by the U.S. Food and Drug Administration with the goal of advancing scientific issues related to the safe and effective use of medical products. She has been recognized by many awards and is an elected member of the National Academy of Medicine. In 2022, she was appointed dean of the UCSF School of Pharmacy.
Talk
Functional Genomics of Transporters: Informing Precision Medicine
To predict the effects of genetic variation on drug response, it is critical to understand the functional effects of rare and common variants. I will describe functional and computational studies focused on coding region variants of OCT1, a transporter that plays a role in human disease and drug response.
Speaker Profile
Biography
Dr Howard McLeod is an internationally recognized expert in precision medicine, having made novel contributions at the discovery, translation, implementation, and policy levels. Dr McLeod has been recognized as a Fellow of both the American Society of Clinical Oncology and the American College of Clinical Pharmacy. He has also been an active Board Member and/or Founder for over a dozen privately held and publicly traded companies. Howard has published over 590 peer reviewed papers on pharmacogenomics, applied therapeutics, or clinical pharmacology and continues to work to advance innovative healthcare.
Session Chair Profile
Biography
Genomics and healthcare leader building clinical and population solutions supporting the healthcare ecosystem. Numerous precision medicine leadership roles in leading health systems, molecular diagnostics, therapeutic development, and genomics/ life science.
Talk
PGx – This Old Dog’s New Tricks
Despite guidelines, technology cost decreases, select EMR integration and payer acceptance – PGx is far from routine care. As the evidence has matured, the market has also evolved with opportunities at the intersection of Value-Based Care and Precision Medicine.This conversation will discuss the field’s progress and opportunity dynamics across stakeholders.
Speaker Profile
Biography
Dr. Tamraz primary interest is identification of genetic determinants of drug response through modern methods aimed at addressing pharmacogenomics research and translating that information into new diagnostics and treatment strategies at point-of-care.
Speaker Profile
Biography
Dr. Schultzs focus in her current position is to provide precision medicine to all patients across a vast rural area. She has been integral to Sanford Healths effort to implement and expand pharmacogenomics into primary care. She serves as Professor of Internal Medicine for the University of South Dakota College of Medicine in 2018. April received her certification of clinical application of pharmacogenomics in 2018 from the University of Florida and serves as a member of the Clinical Pharmacogenomics Implementation Consortium.
Speaker Profile
Biography
Ray currently works at Optum Rx within the Product & Strategy organization. Over the past 4 years he has been charged to explore the space of Pharmacogenomics, and how it could be utilized within the Pharmacy Benefit Manager space. In this work he has helped conduct 4 pilots and 1 clinical study. These studies have been targeted toward answering the companies killer questions. The last of which is what the clinical study was looking to answer, which is will the use of PGx drive down the total cost of care for a utilizing member. Ray has been at UnitedHealth Group for the better part of 15 years with roles Marketing, Research & Development, Operations, and Product Development.
Speaker Profile
Biography
Stirling Bryan is a health economist with a passion for building and supporting patient-oriented learning health systems. Before emigrating to Canada in 2008, Stirling held academic positions in the U.K. at St Thomas’ Hospital, Brunel University, and the University of Birmingham. He was a Commonwealth Fund Harkness Fellow in 2005/06, spending a year at Stanford University, and in 2020 was elected as a Fellow of the Canadian Academy of Health Sciences.